Fungal nail infections, also known as onychomycosis, are more common than you might think. According to the Centre for Disease Control and Prevention, 14% of people worldwide are affected by this condition. It's not just a cosmetic issue; it can significantly impact your quality of life.
Fungal infections cause nails to become brittle, discoloured, and even detach from the nail bed, leading to discomfort and self-consciousness.
The good news? Fungal nail infections are treatable, and taking the right steps can restore your nails to their natural state. In this article, you'll learn about the causes, symptoms, and fungal nail infection treatment, along with practical advice to manage the condition effectively.
Key Takeaways:
- Fungal nail infections are common and can cause nails to become thick, discoloured, or brittle.
- Early treatment is crucial to prevent the infection from worsening or spreading.
- Topical treatments, oral medications, and sometimes nail removal are effective treatment options.
- Proper hygiene, breathable footwear, and avoiding communal areas can help prevent infections.
- Timely medical intervention can ensure the infection is treated effectively before complications arise.
What is a Fungal Nail Infection?

A fungal nail infection happens when fungi get into your nails and cause them to change in appearance. You might notice your nails becoming thicker, discoloured, or even starting to crumble. This infection typically begins with small spots under the nail but can spread if ignored.
Fungal infections are most common in warm, damp environments, like sweaty shoes or shared public spaces such as swimming pools.
With a better understanding of what a fungal nail infection is, let's explore the symptoms that can help you spot it early.
Common Symptoms of Fungal Nail Infections

Fungal nail infections typically start with subtle signs that you may overlook at first. As the infection progresses, however, the symptoms become more noticeable and can cause discomfort. Being aware of these early indicators can help you seek treatment before the infection worsens.
Here are the most common symptoms to watch for:
- Discolouration: The nail may develop white, yellow, or brown spots, often starting at the tip and spreading toward the base. This discolouration is one of the first signs of infection.
- Thickening of the Nail: As the infection progresses, the nail can become thicker and harder to trim, making it uncomfortable to wear shoes or walk properly.
- Nail Crumbling or Brittle Texture: Affected nails may start to crumble, break easily, or appear brittle, causing a rough texture along the surface.
- Distortion in Shape: The nail may become distorted or lift from the nail bed, causing discomfort and making everyday tasks more challenging.
- Foul Odour: In some cases, the affected nail may emit a slight foul smell, indicating a more severe infection that requires prompt attention.
If you notice these symptoms, it's important to act fast. Let's now look at what causes these infections and who is at risk.
Causes and Risk Factors for Fungal Nail Infection

Fungal nail infections are triggered by various fungi, including moulds and yeasts, which thrive in warm, moist environments. Recognising the causes and risk factors can help you take preventive measures to avoid infection. Certain conditions and habits can make you more prone to these infections, so it's important to stay informed.
Here are the key causes and risk factors to consider:
- Fungi, Yeast, and Moulds: The infection is mainly caused by dermatophytes, a type of fungus that feeds on the keratin in nails. Yeasts and moulds can also cause nail infections, especially in individuals with weakened immune systems.
- Warm, Moist Environments: Fungi succeed in warm and damp areas, such as sweaty shoes, damp socks, or communal places like swimming pools and gyms. Wearing closed shoes for long periods can increase your risk, as they create the ideal environment for fungi to grow.
- Age: As you age, your nails grow more slowly, and the circulation in your hands and feet decreases, making older adults more susceptible to fungal nail infections. This also reduces the skin's ability to fight off the infection.
- Diabetes and Immune System Weakness: Individuals with diabetes or weakened immune systems (from conditions like HIV/AIDS or cancer treatments) are more vulnerable, as their bodies struggle to combat infections.
- Previous Nail Injury: If your nails have been injured in the past, even slightly, the damage can create an entry point for fungi. A small break in the nail or cuticle makes it easier for the infection to take hold.
Now that you understand the causes and risk factors, let's take a look at the different types of fungal nail infections.
Different Types of Fungal Nail Infections
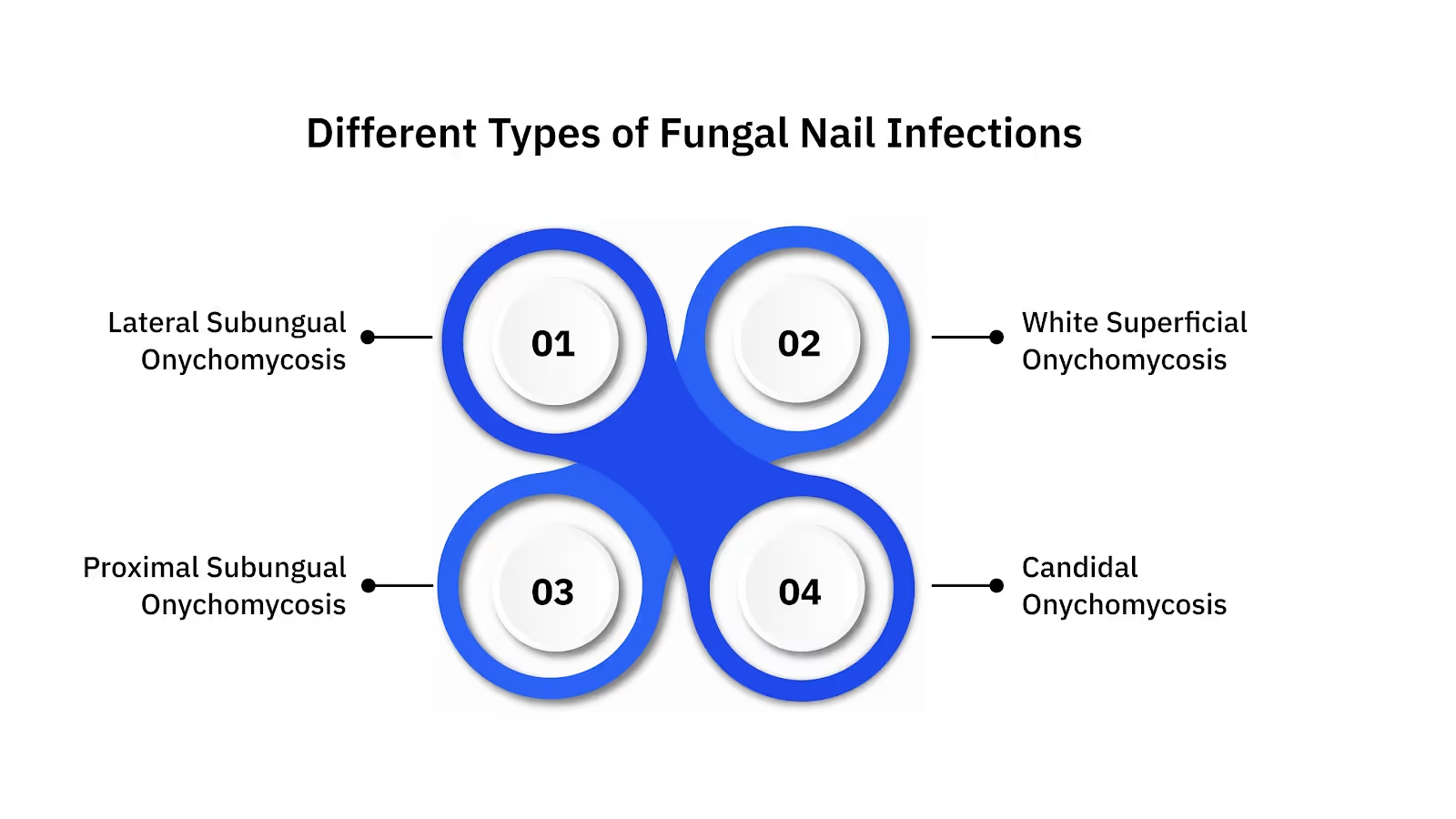
Fungal nail infections can vary in type, affecting different parts of the nail in distinct ways. Understanding the specific type of infection can help determine the most effective treatment. Each type of infection has its own set of characteristics, and some are more severe than others.
Here are the most common types of fungal nail infections:
1. Distal or Lateral Subungual Onychomycosis
This is the most common type of fungal nail infection. It starts at the tip of the nail and works its way towards the base, causing the nail to thicken, discolour, and eventually crumble. It primarily affects the toenails and can be quite painful if not treated.
2. White Superficial Onychomycosis
This type targets the nail's surface, forming white spots that slowly spread across the entire nail. It is less severe than other types but can still cause cosmetic issues and may lead to the nail's eventual destruction if left untreated.
3. Proximal Subungual Onychomycosis
A rarer and more severe form, this type starts at the base of the nail and works upwards. It is more frequently observed in people with weakened immune systems, like those living with HIV or undergoing chemotherapy.
4. Candidal Onychomycosis
Caused by the Candida species of yeast, this infection typically affects fingernails and is more common in people who have frequent exposure to moisture, like dishwashers or healthcare workers. It can cause the nail to become swollen, red, and painful, often with a thickening of the nail.
Also Read: Fungal Infection: Types, Symptoms, and Treatments
Now that you know the different types, let's look into how fungal nail infections are diagnosed.
How is Fungal Nail Infection Diagnosed?

Diagnosing a fungal nail infection involves a thorough examination by a healthcare professional to identify the cause and severity of the infection. Since the symptoms of fungal nail infections can mimic other conditions, a proper diagnosis is essential for effective treatment.
Your healthcare provider may perform specific tests to confirm the infection and rule out other possible causes.
Here's how a fungal nail infection is typically diagnosed:
1. Clinical Examination by a Healthcare Provider
A doctor or dermatologist will begin by inspecting your nails for common signs of a fungal infection, like discoloration, thickening, or crumbling. This first check helps decide if additional tests are necessary.
2. Microscopic Examination
In some cases, your doctor may take a sample from the infected nail and examine it under a microscope. This test helps pinpoint the exact type of fungus or yeast causing the infection.
3. Culture Test
Your doctor may send a sample of the nail debris to a lab for a culture test, which can confirm the presence of fungal organisms. This is the most accurate way to identify the type of fungus causing the infection.
4. KOH Preparation
A potassium hydroxide (KOH) preparation involves placing a small sample of your infected nail in a solution and examining it under a microscope. This test helps identify fungal elements in the nail.
5. Nail Biopsy
In rare cases, if the infection is severe or unresponsive to treatment, your doctor may take a biopsy of the affected nail. This involves removing a small portion of the nail for laboratory analysis to confirm the presence of a fungal infection or rule out other conditions.
Accurate diagnosis ensures that you receive the right treatment to address the infection effectively. Now, let's explore the various treatment options available.
Treatment Options for Fungal Nail Infections

Fungal nail infections can be effectively treated with the right approach. Depending on the severity of the infection, several treatment options are available. Early intervention can improve the chances of recovery, restoring your nails to their natural state.
Here are the most common fungal nail infection treatment options:
- Topical Antifungal Treatments: Medicated nail polishes and creams like ciclopirox and efinaconazole are applied directly to the affected nail. These treatments are most effective for mild to moderate infections and help eliminate the fungus over time.
- Oral Antifungal Medications: For more serious infections, doctors often prescribe oral antifungal medications like terbinafine or itraconazole. These work systemically to target the infection, typically requiring weeks of treatment.
- Nail Removal: If the infection is severe and unresponsive to other treatments, removing the infected nail surgically may be required. This procedure removes the infected tissue and enables a healthy new nail to grow.
- Laser Therapy: Laser treatment uses targeted light to kill the fungi beneath the nail without damaging surrounding tissue. This is an alternative for those who cannot tolerate oral medications or prefer non-invasive treatments.
- Home Remedies and Natural Treatments: While not always as effective as professional treatments, some people use natural antifungal remedies like tea tree oil or vinegar. However, these should not replace prescribed treatments, especially for moderate to severe infections.
Are you struggling with a fungal nail infection that won't go away?
Velantis Dermatology, led by Dr. Janani Sree C M, offers evidence-based treatments to effectively tackle fungal nail infections. Book a Consultation with our MD Dermatologist today and take the first step toward healthier nails!
Preventing and Managing Fungal Nail Infections: The Importance of Timely Treatment and Intervention

Preventing fungal nail infections starts with simple yet effective hygiene practices.Taking preventive measures can lower the chances of developing these infections. Managing an existing infection with timely treatment is equally important to prevent further complications and ensure the infection doesn't spread.
Here are key prevention and management strategies:
- Maintain Good Hygiene: Regularly wash your hands and feet, paying special attention to drying them thoroughly after washing. Fungi grow in moist environments, so keeping your nails dry is essential.
- Wear Breathable Footwear: Opt for shoes that allow air circulation, especially if you wear them for long periods. Avoid wearing damp shoes, as they provide the perfect environment for fungi to grow.
- Avoid Walking Barefoot in Public Areas: In places like swimming pools, gyms, and locker rooms, always wear flip-flops or protective footwear. These public spaces are common breeding grounds for fungi.
- Treat Athlete's Foot Promptly: Athlete's foot can lead to fungal nail infections if left untreated. Use antifungal treatments to manage athlete's foot and prevent it from spreading to your nails.
- Seek Timely Medical Treatment: If you notice signs of a fungal nail infection, such as discolouration or thickening of the nails, it's crucial to seek treatment early. Timely intervention can prevent the infection from worsening and affecting other nails.
Implementing these preventive measures promptly can help minimise the risk of fungal nail infections.
Read Next: Nail Surgery: Procedures, Recovery, and Risks
Conclusion
Fungal nail infections are common but treatable conditions that can cause significant discomfort and self-consciousness if left unchecked. Timely treatment, whether through topical or oral antifungal medications, nail removal, or even laser therapy, can help restore your nails.
Preventing these infections starts with proper hygiene and avoiding communal areas without protection.
Velantis Dermatology, led by Dr. Janani Sree C M, offers expert care for fungal nail infection treatment, ensuring a personalised and scientifically backed approach to your nail health. If you're struggling with a fungal nail infection, Book a call today to consult with our MD Dermatologist and start your treatment journey.
FAQs
Q1. How effective are topical treatments for fungal nail infections?
A1. Topical treatments like medicated polishes and creams can be effective for mild to moderate fungal nail infections. However, they may take several weeks or even months to show noticeable improvements, and their success varies depending on the infection's severity.
Q2. How long does it take to recover from a fungal nail infection?
A2. Recovery time depends on the severity of the infection and the treatment used. With oral antifungal medications, you may start seeing results within 2 to 4 weeks, but full recovery can take up to 6 months, as nails grow slowly.
Q3. Are there any risks associated with using oral antifungal medications?
A3. Oral antifungal medications, while effective, can cause side effects like liver issues or digestive discomfort. It's important to discuss these risks with your doctor before starting treatment, especially if you have underlying health conditions.
Q4. How much does fungal nail infection treatment cost?
A4. The cost of treatment varies depending on the type and severity of the infection. Topical treatments are typically more affordable, while oral medications and laser therapy can be more expensive, with prices ranging from a few hundred to several thousand rupees.
Q5. Can fungal nail infections spread to other nails or parts of the body?
A5. Yes, fungal nail infections can spread to nearby nails or even other parts of the body, such as the skin. It's important to treat the infection promptly to prevent it from spreading and causing further complications.


.png)




