Overview
- What it is: Nail surgery helps fix stubborn ingrown nails, infections, or nail deformities when home treatments don't work.
- Why it helps: Provides lasting relief and prevents repeat problems that over-the-counter solutions can't solve.
- How it's done: A safe procedure under local anaesthesia, removing part or all of the nail if needed.
- What to expect: Minimal pain, walking possible within a day or two, complete healing with simple care in a few weeks.
Dealing with stubborn nail problems, chronic ingrown nails, recurring infections, or uncomfortable deformities can be frustrating and impact daily activities. When home care and common treatments fail to ease the pain, living with these issues can feel never-ending. We understand how discouraging it can be to struggle with persistent nail issues that affect your comfort and confidence, especially when quick fixes don't help.
For many, nail surgery becomes a safe, medically recommended step to address the underlying cause and bring lasting relief. It's not just about appearance; it's a precise, minor procedure performed under local anaesthesia to restore comfort and function.
This overview explains when nail surgery is considered, what to expect during the procedure, and how recovery works. Understanding each step can help anyone struggling with persistent nail conditions make informed choices and look forward to healthier, pain-free nails.
What is Nail Surgery?
Nail surgery is a precise, medically recommended procedure that directly addresses persistent nail issues, providing a more permanent solution than topical treatments, which often only offer temporary relief.
Once the underlying condition is evaluated correctly, the procedure may include techniques such as partial or complete nail removal, taking a small tissue sample (biopsy) to diagnose unusual lesions, or surgically altering the nail's structure to restore normal growth and comfort. By addressing the root cause, nail surgery provides a lasting solution for chronic or complex nail disorders.
Why Patients Consider Nail Surgery?
Chennai residents often seek nail surgery after experiencing recurring problems despite their consistent efforts at self-care. The procedure addresses structural issues that conservative treatments cannot resolve, providing definitive solutions for chronic conditions.
Conditions that Require Nail Surgery

Several nail conditions warrant surgical intervention when conservative treatments prove insufficient. The following conditions commonly require nail surgery for effective resolution:
- Persistent ingrown toenails that cause chronic pain, redness, or infection often require nail surgery when home treatments fail to provide relief.
- Severe fungal infections can lead to thickened, deformed nails that may require nail surgery when medications alone are no longer effective in restoring a standard structure and appearance.
- Severe nail trauma can require surgical treatment to prevent complications and support healthy regrowth of new nail tissue.
- Suspicious lesions with abnormal pigmentation or growth beneath the nail may need a surgical biopsy to diagnose conditions such as melanoma through detailed tissue analysis.
- Chronic paronychia that does not resolve with antibiotics may benefit from partial nail surgery to remove the source of repeated infection and inflammation.
- Pronounced pincer nails that are excessively curved or deformed can be surgically reshaped to improve function and relieve persistent pain.
At Velantis Dermatology in Chennai, we follow proven methods and maintain a clean, safe environment to make sure you get the best possible results.
7 Common Types of Nail Surgery Procedures
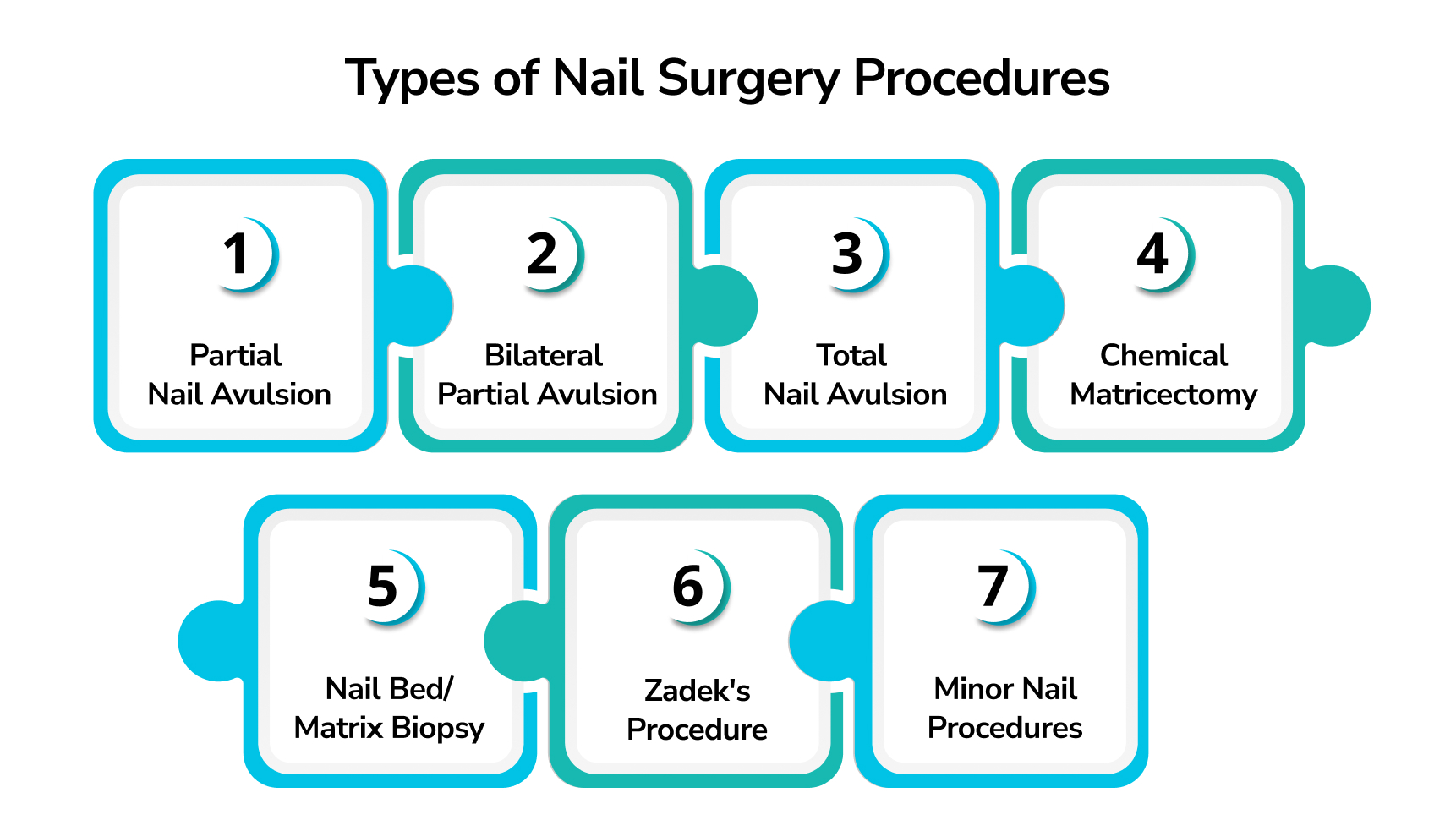
Nail surgery involves carefully removing affected nail tissue and treating the nail matrix based on the specific condition to resolve issues while reducing risks effectively.
The choice of procedure depends on factors like nail thickness, infection severity, previous treatment failures, and patient-specific considerations. Complications can be minimised by implementing preventive measures, such as careful patient selection, sterile technique, and gentle treatment of the nail matrix.
1. Partial Nail Avulsion (Wedge Resection)
Partial nail avulsion carefully removes the problematic nail strip while preserving healthy tissue, followed by treatment of the nail matrix with chemicals such as phenol or cautery to prevent regrowth. This approach offers high success rates and long-term relief with minimal recovery time.
2. Bilateral Partial Avulsion
Bilateral partial nail avulsion removes narrow wedge-shaped sections from both sides of the nail for double-sided ingrown toenails. It preserves the healthy central part and maintains a natural appearance, while treating both nail matrices to prevent regrowth and provide long-term relief without the need for multiple surgeries.
3. Total Nail Avulsion
Total nail avulsion involves complete removal of the entire nail plate in cases of severe infection, deformity, or damage, exposing the nail bed for comprehensive treatment and cleaning, combined with matrix treatment using chemical or surgical methods to prevent regrowth.
Studies show that total nail avulsion with matrix management can be safely performed in a standard dermatology clinic with minimal specialised equipment, ensuring this comprehensive treatment remains accessible and practical for patients who need complete resolution of stubborn nail conditions.
4. Chemical Matricectomy
Chemical matricectomy involves using an 88% phenol solution or electrocautery to permanently destroy nail matrix cells in targeted areas, effectively preventing nail regrowth.
Dermatologists apply this chemical treatment after partial or total nail surgery to ensure definitive results. Clinical studies demonstrate that phenol cauterisation offers excellent outcomes with minimal recurrence rates when performed correctly.
5. Nail Bed/Matrix Biopsy
Diagnostic nail surgery involves collecting small tissue samples from the nail bed or matrix under local anaesthesia. This procedure diagnoses suspicious nail lesions, including melanoma, psoriasis, tumours, and other nail diseases.
The biopsy may require partial nail removal for proper access to underlying tissues. Medical literature emphasises that nail organ avulsion is essential for identifying malignant diseases, drug side effects, and bacterial infections beyond common onychomycosis.
6. Zadek's Procedure
Zadek's procedure represents the most comprehensive approach to nail surgery, involving the complete removal of the nail with total matrix excision. This aggressive treatment addresses severe recurrent cases or situations where multiple previous therapies have failed.
Complete matrix removal ensures permanent resolution of chronic nail problems.
7. Minor Nail Procedures
The minor nail procedures usually consist of:
- Subungual Hematoma Drainage: Emergency nail surgery relieves trapped blood under the nail by drilling a small hole to release pressure. This trauma-related procedure preserves the nail plate while addressing acute blood accumulation beneath.
- Nail Fold Repair: Surgical repair addresses damaged nail fold or bed structures following extensive tumours, severe injuries, or structural damage. Studies show that proper technique and post-operative care significantly reduce the risk of infection following nail surgery procedures.
How to Prepare for Nail Surgery
Before nail surgery, a few critical preparations ensure a safe and smooth experience. These steps align with Velantis Dermatology's commitment to evidence-based, doctor-led care, ensuring predictable outcomes rather than quick fixes.
1. Stop smoking & manage underlying conditions.
Quitting smoking is essential as it delays wound healing and increases complications; additionally, optimising diabetes control and blood thinner levels promotes faster healing and smoother recovery.
2. Understand your procedure
During the consultation, your dermatologist will explain the exact method—partial nail avulsion, total removal, or chemical matrixectomy—and set realistic expectations. A digital nerve block is standard for nail surgery, providing effective numbing with minimal trauma. Controlling bleeding effectively during surgery helps prevent complications and promotes a cleaner, faster healing process.
3. Day‑of‑Surgery Tips
Choose open-toed or loose shoes to protect the surgical site and avoid tight footwear. Arrange for someone to drive you home, as driving right after isn't recommended. Rest at home, keep the foot elevated, and leave the initial dressing intact.
The Nail Surgery Procedure: Step-by-Step
Begin by addressing nail issues with conservative methods such as proper trimming, topical antifungal treatments, or oral medications. Surgical treatment is recommended if these symptoms do not resolve or persistently cause pain, infection, or nail deformity. Nail surgery involves a careful process: confirming the diagnosis, selecting the most appropriate surgical approach, and performing the procedure in a sterile environment to minimise risks and promote proper healing.
Step 1. Pre-Operative Phase
The pre-operative phase consists of :
- Initial Consultation and Assessment: A clinical examination reveals the severity of nail involvement and the patterns of surrounding tissue inflammation. Our dermatologist assess nail plate thickness, the extent of infection, and tissue viability before recommending surgical intervention. A medical history review identifies diabetes, blood-thinning medications, or allergies that may complicate the healing process.
- Discussion covers realistic expectations, including healing timelines and potential recurrence rates. Informed consent addresses all risks, benefits, and alternative treatments available for nail surgery candidates.
- Preparation for Surgery: Antiseptic cleaning with chlorhexidine kills surface bacteria while preserving skin integrity. Sterile draping creates a contamination-free environment essential for successful nail surgery. A tourniquet applied at the base of the finger or toe temporarily reduces blood flow to control bleeding and improve surgical visibility; it must be monitored closely to avoid tissue damage and patient discomfort.
Step 2. Anaesthesia and Pain Management
This part of the procedure involves :
Local Anaesthetic Administration: Before a nail surgery begins, a local anaesthetic is used to numb only the surgical site while the patient remains fully awake. Regional anaesthesia involves carefully injecting a numbing medicine, usually lidocaine, near the base of the affected toe or finger. This digital block prevents pain signals, ensuring a painless procedure. Typically, numbness develops within 5–10 minutes and lasts 2–3 hours after surgery, covering the entire treatment comfortably in about 95% of cases.
- A tourniquet applies controlled pressure to stop bleeding without cutting off blood flow entirely, with careful monitoring to ensure patient comfort and prevent tissue damage.
Step 3. The Surgical Procedure
This phase involves meticulous surgical steps, including maintaining a sterile environment, carefully removing the affected nail portions, and treating the nail matrix to prevent regrowth.
- Sterile Technique Protocol: This technique involves thorough instrument sterilisation and maintaining a sterile field during surgery to prevent infections and reduce post-operative complications effectively.
- Nail Removal Process: Partial avulsion removes only diseased nail portions, preserving healthy tissue and minimising recovery time. Total avulsion addresses severe cases requiring complete nail removal for optimal healing. Specialised instruments, including nail elevators, surgical scissors, and scalpels, ensure precise tissue handling during nail surgery procedures.
Nail Matrix Treatment: Applying phenol for 30-60 seconds chemically destroys the nail matrix cells responsible for nail growth, effectively preventing regrowth in most cases and reducing the chances of the problem recurring.
Step 4. Post-Procedure Care
Immediate Post-Operative Steps are as follows:
- Tourniquet removal requires careful assessment of bleeding and confirmation of hemostasis before dressing application.
- Sterile gauze dressing with compression bandaging controls minor bleeding for the first 24 hours following nail surgery.
Recovery Process After Nail Surgery
Recovery after nail surgery requires careful wound care and adherence to activity restrictions. Understanding the recovery timeline and proper protocols helps patients set realistic expectations and minimise the risks of complications, promoting optimal healing.
What to Expect Immediately After Surgery?
Following nail surgery, patients can typically walk immediately or the next day, but should limit movement and rest with foot elevation for 1-2 days. Complete healing takes 4-6 weeks, with regular dressing changes and prescribed pain management, excluding aspirin unless otherwise advised.
Dressing Care and Wound Management
Keep the initial bandage in place for 24-48 hours after the procedure, ensuring it remains completely dry. After removing the bulky dressing, begin daily dressing changes using sterile bandages. Clean the wound gently with mild soap and water, pat dry, and apply fresh dressing materials as instructed. Change dressings every 2 days, keeping the wound dry on alternate days to promote healing.
Bathing and Hygiene Tips
Avoid getting the surgical site wet for the first 48 hours after nail surgery. Once initial dressings are removed, you can shower while protecting the wound area. Allow controlled water exposure during dressing changes, but avoid prolonged soaking until the wound has progressed significantly.
Activity and Footwear Precautions
Walking is generally allowed right after the procedure, but activity should be kept minimal during the first two days to support healing. High-impact movements, such as running, gym workouts, or wearing tight footwear, should be strictly avoided for at least 1–2 weeks post-surgery. During this period, opt for open sandals or spacious shoes that place no pressure on the treated area. After 2–3 weeks, you can gradually shift to loose-fitting, closed-toe shoes, depending on your comfort and the progress of your healing.
However, in cases of total nail avulsion, longer recovery is necessary—patients may need to limit activity and avoid enclosed footwear for up to 4–6 weeks to allow the nail bed to heal fully.
Healing Timeline and Nail Regrowth
Initial healing of the nail bed usually occurs within 7-10 days, with full recovery ranging from 3 to 6 months, depending on the procedure. Partial nail removal often leads to regrowth within 3-4 months, whereas complete removal can take up to a year.
Follow-Up Visits and Monitoring
Schedule your post-surgery check-up within one week to assess healing progress. Your dermatologist will examine the site for signs of infection, abnormal regrowth, or delayed healing. Contact your clinic immediately if you notice increasing pain, swelling, excessive discharge, or red streaking around the wound.
Long-Term Considerations
Possible Nail Regrowth
Partial nail regrowth can occur if some nail matrix tissue remains after surgery; in such cases, a repeat procedure may be required for permanent correction.
Lifestyle & Nail Care
Trim nails straight across to prevent future ingrown edges. Choose properly fitted footwear that doesn't compress toes. Perform regular self-examinations for early signs of recurrence and consult your dermatologist promptly if problems arise.
What Makes Velantis Dermatology a Trusted Choice for Nail Surgery?

When considering nail surgery, choosing the right medical provider is crucial for both safety and successful outcomes. Velantis Dermatology combines medical expertise with state-of-the-art facilities to deliver comprehensive nail surgery services that patients can trust.
Doctor-led, Sterile Protocols
All nail surgery procedures at Velantis Dermatology are performed by qualified dermatologists following strict sterile protocols. Our surgical suite maintains hospital-grade standards with proper sterilisation equipment, sterile instruments, and controlled environments to minimise infection risk. Each procedure follows established medical guidelines, comprehensive pre-operative assessment, and post-operative care instructions.
Specialising in Complex Nail Cases
Our dermatologist have extensive experience managing complex nail conditions, including severe ingrown nails, recurrent infections, nail tumors, and chronic deformities. We assess each case carefully, considering underlying issues such as diabetes or circulation problems that might affect healing. This specialized approach enables us to handle cases needing referral to other specialists.
Advanced Techniques Like Phenolisation and Matrix Excision
We use proven surgical techniques, including chemical phenolisation for permanent nail border removal and precise matrix excision procedures. Phenolisation involves applying phenol to destroy nail-producing cells, preventing regrowth of problematic nail segments. Matrix excision offers surgical removal of specific nail matrix areas when conservative treatments have failed. These techniques are chosen based on individual patient anatomy and the severity of their condition.
High Patient Success Rate
Our systematic approach to nail surgery consistently achieves positive outcomes with minimal complications. Success is measured by complete symptom resolution, proper healing without infection, and patient satisfaction with functional results. We keep detailed records of treatment outcomes and continuously monitor healing progress through scheduled follow-up appointments.
Pain Management and Safety
Modern nail surgery uses effective pain control techniques that minimise discomfort. Explaining what to expect can help reduce common fears and misunderstandings about nail surgery.
Pain Control During and After Surgery
Nail surgery is performed under local anaesthesia (like lidocaine or ropivacaine), numbing the area after a brief sting so the procedure is virtually painless; patients remain awake and typically experience mild, manageable post-operative discomfort that can be controlled with over-the-counter pain relievers like paracetamol.
When to Seek Medical Attention Post-Surgery
Monitor for these warning signs after nail surgery:
- Infection Signs: Spreading redness beyond the operated area, increasing pain or swelling, yellow/green discharge, or fever ≥38°C.
- Heavy Bleeding: Blood soaking through multiple dressings despite rest
- Severe Pain: Sudden worsening pain not relieved by prescribed medication
- Allergic Reactions: Hives, rash, or breathing difficulties after medications
- Non-Healing Wound: No improvement or worsening after 2-3 weeks
Contact your doctor immediately if you notice heat, swelling, or increasing pain, as these may indicate an infection that requires prompt antibiotic treatment. Velantis offers medically supervised post-surgical follow-up for timely evaluation and appropriate care to ensure safe recovery and early intervention if needed.
Potential Risks and Complications
Potential risks associated with nail surgery include mild bleeding, swelling, and discomfort. Closely monitoring for infection and following sterile techniques and proper wound care significantly reduce these risks.
Specific complications may include infection, delayed healing, allergic reactions to anaesthetics, or regrowth of the nail if the matrix is incompletely treated. Rare outcomes may consist of minor scarring or nail deformities, making awareness essential for proper aftercare and timely medical consultation.
Specific Procedure-Related Risks
The following are a few procedure-related risks:
- Infection is a primary concern post-surgery.
- Patients should be vigilant for symptoms that warrant medical attention.
- Some bleeding is normal; however, excessive bleeding should prompt a call to your doctor.
- Delayed healing can occur, particularly with chemical ablation techniques.
- Nerve injury is a sporadic risk, but can lead to numbness from local anaesthetics.
- Other potential issues include:
- Redness and inflammation, caused by a phenol flare, is a temporary localised skin reaction after phenol application in nail surgery, which generally resolves on its own without needing treatment.
- Expected mild pain
- Possibility of scarring or nail deformity
- Recurrence of nail problems may happen if the nail matrix isn't destroyed, necessitating repeat surgery.
How to Minimise Risks and Complications
To minimise risks associated with nail surgery, it is essential to use evidence-based surgical techniques, including precise matrix treatment, a strict sterile protocol, and individualised risk assessments for patients with diabetes or those taking blood thinners, to reduce the risk of infection.
Understanding these potential complications and how to mitigate them is vital for anyone considering nail surgery. As we delve deeper into the topic, the next section will explore the cost considerations in Chennai, providing a comprehensive view of what to expect financially when undergoing nail surgery.
Cost Considerations in Chennai
Nail surgery provides precise treatment for chronic nail problems such as ingrown toenails, with services in Chennai focusing on evidence-based care, transparency, and ethical practises.
Typical Cost Range
In Chennai, nail surgery for ingrown toenails typically costs between ₹2,000 and ₹5,000, though prices can vary depending on the clinic and the complexity of the procedure. When more extensive treatment is necessary like total nail removal, costs can increase to ₹15,000-₹30,000.
Various factors influence the price, including the extent of the surgery, the type of anaesthesia used, postoperative dressings, and the level of follow-up care. Clinics with advanced medical facilities or experienced dermatologists may charge more, reflecting the quality and safety of their care.
For patients seeking trustworthy guidance and transparent, medically supervised treatment, Velantis offers evidence-based nail surgery focused on clinical accuracy and patient-centred care.
Insurance and Payment
Nail surgery is usually an outpatient procedure, not covered by insurance in India, so patients typically pay out of pocket.
This financial clarity empowers Chennai residents to plan nail surgery confidently, addressing chronic pain effectively. We'll break everything down into key conclusions to guide your decision-making process.
Conclusion
When performed by a skilled dermatologist, nail surgery lowers the risk of complications, recurrence, or scarring and helps rebuild confidence and comfort over time. Opting for doctor-led care instead of quick fixes allows patients to manage chronic nail conditions safely and effectively, resulting in better outcomes without false promises or cosmetic hype.
Unlike over-the-counter remedies or unqualified treatments, which often fail and lead to repeated infections or nail deformities, proper nail surgery provides lasting results through structured, evidence-based care.
The key to successful nail surgery lies in choosing an experienced dermatologist who prioritises sterility and ethical practices. Patients benefit from clear explanations of the procedure, including what to expect during recovery and how to manage pain effectively. Recovery timelines vary, but with proper aftercare, most individuals resume normal activities quickly while maintaining healthy nails.
If you're facing repeated nail problems and seek safe, long-lasting solutions, schedule a consultation with Velantis today. Our dermatologist offer personalised, ethical, and evidence-based nail surgery aimed at genuine recovery, not quick fixes.
FAQs
Q1. Is Nail Surgery Painful?
A1. Nail surgery is performed under local anaesthesia, which causes a quick sting but effectively numbs the area, ensuring the procedure is pain-free. Any mild discomfort afterwards is typically manageable with common pain relievers like paracetamol.
Q2. How Long Is Recovery?
A2. Most patients can walk and perform light activities the day after nail surgery, with rest and foot elevation recommended for 1-2 days; complete healing typically takes 4-6 weeks with regular dressing changes for proper recovery.
Q3. Will My Nail Grow Back?
A3. If only part of the nail is removed, the remaining nail may grow back normally, though the treated edge might not. If the nail matrix is entirely removed, the nail won't regrow. Regrowth occurs in less than 5% of cases.
Q4. Can Home Care Avoid Surgery?
A4. Mild ingrown toenails may improve with warm soaks and proper nail trimming. However, chronic or infected cases often require nail surgery for a permanent solution, as home remedies may only provide temporary relief.
Q5. How Do I Care for My Toe/Finger After Surgery?
A5. Keep the area clean and dry, following your doctor's dressing change instructions. Soak the toe in warm water and apply antibiotic ointment as advised. Avoid tight shoes to prevent irritation during healing.
Q6. Is Nail Surgery Safe for Diabetics?
A6. Nail surgery is generally safe for diabetic patients if blood sugar is well-controlled. Inform your dermatologist about your condition and medications to ensure proper care and minimise infection risks.
Q7. Is It Safe for Children or the Elderly?
A7. Nail surgery can be performed on children with parental consent and careful explanation to reduce anxiety. It's typically safe for older adults, but overall health must be assessed to avoid complications.
Q8. How Can I Prevent Future Nail Issues?
A8. Cut nails straight across, avoid trimming too short, and wear well-fitting shoes. Keep feet dry to prevent skin softening around nails. Regular podiatrist visits can help if you're prone to issues.


.png)




